Is I‑CBT Right for Me? Signs This OCD Approach Might Be a Good Fit
- Ryan Burns

- Dec 3, 2025
- 7 min read

OCD can make you feel trapped in loops of doubt, mental review, and “What if…?” worries. I‑CBT therapy for OCD (Inference‑Based Cognitive Behavioral Therapy) goes upstream—working directly with the reasoning patterns that fuel obsessional doubt, rather than relying on deliberate exposure exercises. Below, we’ll clarify what I‑CBT is designed to help with, how to tell if it fits your needs, when other options (like ERP or medication) are recommended, and how to explore online I‑CBT in Tennessee at ScienceWorks.
🧠 Key takeaway: Many people who feel stuck in internal compulsions—rumination, mental checking, seeking certainty—find I‑CBT’s reasoning‑first approach intuitive and less overwhelming than exposure‑heavy care (1,2).
🧭 Key takeaway: Evidence suggests I‑CBT is an effective option for OCD and is often better tolerated than standard CBT with ERP, though recent research found non‑inferiority to CBT is still inconclusive (effective, but not yet proven equivalent) (1).
🧩 Key takeaway: You don’t have to choose just one path. Many clinicians combine I‑CBT with ERP, ACT, or medication when that mix better matches your symptoms and goals (3,4).
Natural next steps are to skim the signs below, then bring your questions to a consult. If you’d like to talk it through, you can read more about I‑CBT for OCD in Tennessee and book a call from our page, I‑CBT for OCD in Tennessee.
What I‑CBT Is Designed to Help With
I‑CBT (also called Inference‑Based Therapy or IBT) targets the reasoning style that underlies obsessive doubt—what researchers call inferential confusion: treating a possibility as if it were reality, then acting as though the feared story must be true (5). Instead of asking you to touch doorknobs or face triggers right away, I‑CBT helps you:
Spot how OCD builds a convincing “OCD story” from imagined risk rather than present‑moment evidence (5).
Re‑establish trust in your senses, memory, and common sense—so your decisions rely more on reality than on “what if?” (1,5).
Practice everyday “reality checks” that gently weaken the OCD story without white‑knuckling through exposures (1,5).
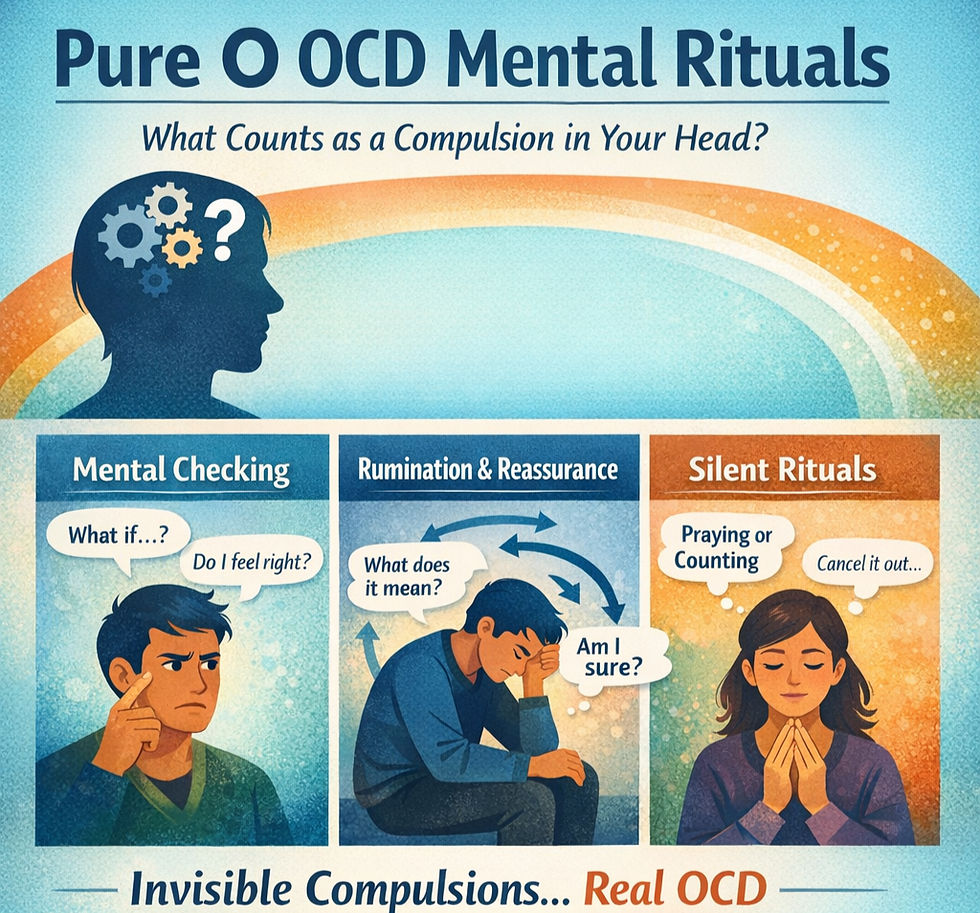
OCD driven by doubt, “What if?”, and mental review
If your compulsions are mostly in your head—rumination, reviewing conversations, mentally checking if you felt “just right,” endlessly seeking certainty—I‑CBT squarely targets those loops (2,4,5). Many clients report that mapping the OCD story, then choosing a more reality‑anchored story, reduces the urge to check or confess.
Situations where outward compulsions are less obvious
I‑CBT can also fit when loved ones don’t notice obvious rituals, but you spend hours internally neutralizing distress (covert reassurance, analyzing, “neutralizing” images). The focus on reasoning lets you work at depth even when exposures feel mismatched or too blunt at first (2,4).
Common Signs You Might Resonate with I‑CBT Therapy for OCD
Feeling stuck in checking, rumination, or seeking certainty
Do you replay scenarios on loop to feel 100% sure? I‑CBT treats certainty‑seeking as part of the OCD story. You practice choosing sufficient evidence over perfect certainty—freeing up time and energy (5).
Having trouble trusting your senses or memory
I‑CBT includes exercises to rebuild trust in your senses and memory—especially helpful when you doubt what you saw, did, or felt (1,5).
Feeling like the threat is in your mind more than in the world
If the danger feels mostly internal (thoughts/images/urges) rather than about external contaminants or locks, I‑CBT’s cognitive emphasis may feel like a better doorway into change (2,4).
When I‑CBT Might Not Be the First or Only Approach
Situations where ERP, medication, or other supports are needed
CBT with Exposure and Response Prevention (ERP) remains a gold‑standard treatment for OCD symptoms across subtypes (6). For some people—especially when compulsions are very behavioral (e.g., visible checking/washing) or when symptoms are severe—ERP and/or medication may be the first recommendation (7). Telehealth ERP also shows good outcomes, which means distance doesn’t have to be a barrier (8,9).
Why professionals sometimes recommend a combination
A good plan matches methods to maintainers. Many clinicians blend I‑CBT’s doubt‑focused tools with ERP’s learning‑through‑doing, or add ACT skills, sleep care (if insomnia is present), and—when appropriate—medication. This is common when insight is poor, rituals are time‑consuming, or distress is high (2,3,4,7). You can explore ERP basics here: A gentle introduction to ERP therapy for OCD on our site.
Questions to Ask Yourself About Fit
How you feel about exposure exercises vs reasoning work
Some people like hands‑on learning (ERP right away). Others prefer starting with reasoning (I‑CBT) until doubt loosens its grip. Both are valid. Ask yourself: Which path would help me start and stick with treatment?
What kind of support helps you feel safer and more empowered
Do you benefit from structured mapping and language for your OCD story? Do you want skills that reduce rumination at work or before sleep? Those are I‑CBT sweet spots. If you’re energized by behavioral experiments and practicing “not doing” compulsions in the moment, ERP may be a strong anchor—possibly alongside I‑CBT.
Questions to Ask a Therapist About I‑CBT
How they decide if I‑CBT is appropriate
How do you assess whether my compulsions are primarily mental vs behavioral?
What signs tell you to start with I‑CBT, blend it with ERP, or pivot to other options?
How will we measure progress (e.g., time spent ruminating, confidence in memory, Y‑BOCS scores)?
How they adjust for trauma, neurodivergence, or complex situations
What changes do you make for autism/ADHD (e.g., pace, sensory needs, structure)?
How do you adapt I‑CBT if I’ve had trauma or medical stressors, or if I mask a lot?
What’s your plan if symptoms spike or insight drops during care?
Safety Considerations and Getting the Right Level of Care
Why it’s important not to DIY treatment for severe OCD themes
It’s normal to read up on strategies. But when obsessions involve self‑harm, harm to others, or intense moral/safety themes, DIY protocols can backfire. A licensed clinician can help you right‑size the plan, monitor risk, and coordinate supports. If you’re in crisis, call 988 (U.S.) or 911.
When to look for a higher level of care or urgent support
If outpatient therapy isn’t enough—because rituals take up many hours per day, you’re missing school/work, or safety is a concern—programs like Intensive Outpatient (IOP) or Partial Hospitalization (PHP) for OCD may be appropriate (10). Your therapist can help you decide if that step is needed and where to go locally.
Exploring I‑CBT for OCD in Tennessee and Online
How to bring up I‑CBT in a consultation call
You could say: “My compulsions are mostly mental—rumination and checking for certainty. I’m curious about starting with I‑CBT or blending it with ERP. What would that look like for me?” If you’d like, start with our page “I‑CBT for OCD in Tennessee” to see how we structure care and what a consult covers.
Options for telehealth I‑CBT if you live in Tennessee
ScienceWorks provides telehealth I‑CBT and ERP‑informed CBT for adults and older teens physically located in Tennessee. You can also read about how we approach I‑CBT for “just‑right” OCD and mental rituals. We’re a neurodivergent‑affirming practice, and we tailor care to your goals and learning style. Explore:
OCD Therapy at ScienceWorks (our overview of approaches and fit)
Specialized Therapy (how we individualize care)
Psychological Assessments (when clarity would help your plan)
Meet the Team (get to know your potential therapist)
Contact Us (ask a question or request a consult)
FAQs
Does I‑CBT replace ERP?
Not necessarily. Some people do very well with I‑CBT alone; others benefit most from a blend with ERP or medication (1–4,7). Your plan should match your symptoms and values.
Can I do I‑CBT online?
Yes—telehealth delivery is common. Even within OCD research during the pandemic, portions of I‑CBT and CBT were successfully delivered via video without harming outcomes (1). ERP over secure video has growing evidence as well (8,9).
Next Steps at ScienceWorks
If you’re looking for an OCD therapist in Tennessee who can tailor a plan using I‑CBT, ERP‑informed CBT, ACT, or a combination, explore these pages:
References and Citations
(1) Wolf, N., van Oppen, P., Hoogendoorn, A. W., van den Heuvel, O. A., van Megen, H. J. G. M., Broekhuizen, A., Kampman, M., Cath, D. C., Schruers, K. R. J., van Es, S. M., Opdam, T., van Balkom, A. J. L. M., & Visser, H. A. D. (2024). Inference‑Based Cognitive Behavioral Therapy versus Cognitive Behavioral Therapy for Obsessive‑Compulsive Disorder: A Multisite Randomized Controlled Non‑Inferiority Trial. Psychotherapy and Psychosomatics, 93(6), 397–411. https://doi.org/10.1159/000541508
(2) Aardema, F., O’Connor, K., Corrigan, K., Pélissier, M.‑C., Leblanc, V., Raheb, H., Nguyen, S., Halili, S., Baribeau, M., Audet, J.‑S., & Van Oppen, P. (2022). Evaluation of Inference‑Based Cognitive‑Behavioral Therapy (I‑CBT) for Obsessive‑Compulsive Disorder: A Multicenter Randomized Controlled Trial. Psychotherapy and Psychosomatics, 91(5), 348–362. https://doi.org/10.1159/000525935
(3) Visser, H. A. D., van Megen, H. J. G. M., van Oppen, P., Eikelenboom, M., Hoogendoorn, A. W., Kaarsemaker, M., & van Balkom, A. J. L. M. (2015). Inference‑Based Approach versus Cognitive Behavioral Therapy in the Treatment of Obsessive‑Compulsive Disorder with Poor Insight: A 24‑Session Randomized Controlled Trial. Psychotherapy and Psychosomatics, 84(4), 254–265. https://doi.org/10.1159/000367928
(4) Aardema, F., O’Connor, K., Delorme, M.‑E., Audet, J.‑S., Bastien, M., Bouchard, C., & Pélissier, M.‑C. (2017). The Inference‑Based Approach (IBA) to the Treatment of Obsessive‑Compulsive Disorder: An Open Trial Across Symptom Subtypes and Treatment‑Resistant Cases. Clinical Psychology & Psychotherapy, 24(5), 1157–1171. https://doi.org/10.1002/cpp.2024
(5) Julien, D., O’Connor, K., & Aardema, F. (2016). The inference‑based approach to obsessive‑compulsive disorder: A comprehensive review of its etiological model, treatment efficacy, and model of change. Journal of Affective Disorders, 202, 187–196. https://doi.org/10.1016/j.jad.2016.05.060
(6) Reid, J. E., Laws, K. R., & Drummond, L. (2021). Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive–compulsive disorder: A systematic review and meta‑analysis. Comprehensive Psychiatry, 107, 152240. https://doi.org/10.1016/j.comppsych.2021.152240
(7) National Institute for Health and Care Excellence (NICE). (2005, last reviewed 2024). Obsessive‑compulsive disorder and body dysmorphic disorder: Recognition and management (CG31). https://www.nice.org.uk/guidance/cg31
(8) Vogel, P. A., Launes, G., Moen, E. M., Solem, S., Haland, Å. T., Hansen, B., & Himle, J. A. (2014). A pilot randomized controlled trial of videoconference‑based ERP for OCD. Journal of Anxiety Disorders, 28(2), 162–170. https://doi.org/10.1016/j.janxdis.2013.09.012
(9) Fletcher, T. L., Fortney, J. C., Curran, G. M., et al. (2021). A pilot open trial of video telehealth‑delivered exposure and response prevention for obsessive‑compulsive disorder in rural Veterans. Frontiers in Psychiatry, 12, 631136. https://doi.org/10.3389/fpsyt.2021.631136
(10) International OCD Foundation (IOCDF). (n.d.). SCP OCD & Anxiety Intensive Outpatient Program (example of IOP level of care). https://iocdf.org/clinics/scp-ocd-and-anxiety-intensive-outpatient-program/
Disclaimer: This article is for informational purposes only and is not a substitute for professional diagnosis or treatment.