ERP Techniques and Real-Life Examples: What ERP for OCD Actually Looks Like
- Ryan Burns

- Nov 26, 2025
- 7 min read

What Is ERP and How Does It Help OCD?
The core idea: facing fears without rituals
Exposure and Response Prevention (ERP) is a behavioral therapy that invites you to face triggers (exposure) while intentionally not doing compulsions or safety behaviors (response prevention). Over time, your brain updates its predictions: intense alarm fades, urges lose their power, and life opens back up. ERP grew from decades of research on exposure learning and emotional processing (5). In multiple meta‑analyses, ERP (usually delivered within CBT) produces large, durable improvements in OCD symptoms, often comparable to or better than medication alone (1, 2).
🔁 Key takeaway: The magic isn’t the exposure itself—it’s not doing the ritual afterward. That’s how new learning sticks.
Why ERP is considered a gold‑standard treatment
International guidelines (NICE; APA) recommend CBT with ERP as a first‑line psychotherapy for OCD across age groups (3, 4). Recent reviews continue to affirm strong effects for ERP across delivery formats, including outpatient and intensive programs (2, 6).
For clients in Tennessee and beyond, ERP can also be delivered securely via telehealth, with growing evidence for feasibility, acceptability, and symptom improvement (7, 8, 9).
🌐 Key takeaway: Yes, online ERP therapy can work—especially when sessions include real‑life, at‑home exposures guided in real time.
Key Parts of Exposure and Response Prevention
Exposure to feared thoughts, images, and situations
Exposures are planned practices that bring on the thoughts, sensations, or situations your OCD tells you to avoid. Depending on your goals, exposures may involve:
Situations (touching doorknobs; leaving appliances unplugged;sending a text without rereading twelve times)
Cues and images (looking at a triggering photo; writing a provocative sentence)
Internal triggers (noticing an urge; inviting a “what if?” thought on purpose)
Underneath, we’re targeting learning—teaching your brain that the feared outcome is less likely than OCD claims and that anxiety can rise and fall without rituals (5, 6).
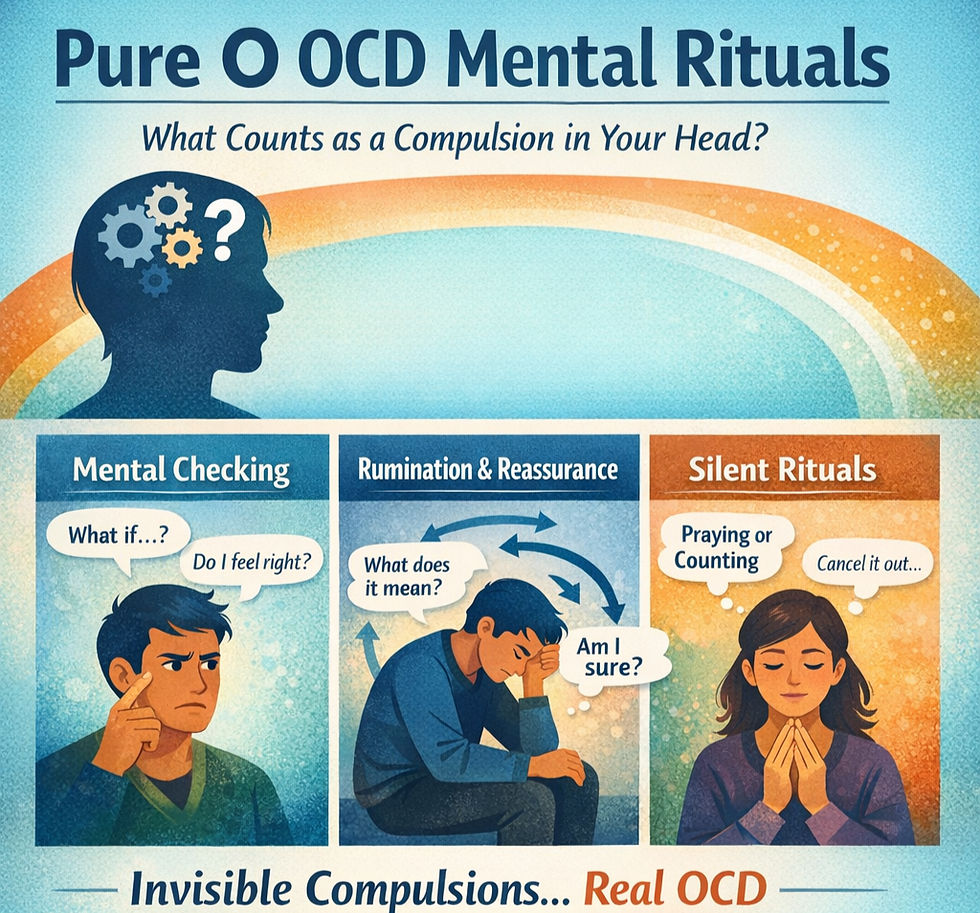
Response prevention and dropping safety behaviors
Response prevention means not doing compulsions and dropping subtle safety behaviors that sneakily “take the edge off,” like seeking reassurance, praying to undo, scanning your body, or counting. We plan in advance what you’ll not do during an exposure and how you’ll ride out urges. Over time, your nervous system recalibrates; you gain freedom to act by choice rather than by compulsion (1, 2, 6).
🛑 Key takeaway: If you keep a “tiny ritual” just in case, your brain keeps the old alarm file open. Close the file by not doing it.
Common ERP Techniques in Therapy
In vivo (real‑life) exposures
These are real‑world practices done during or between sessions. Examples:
Touch a public doorknob and delay hand‑washing for a set time
Leave the house with the stove unchecked
Send an email with a minor, planned typo and resist rereading
Walk past a church without performing a neutralizing prayer
Why it works: Real‑life exposures create powerful learning because they match your everyday triggers and consequences (6).
Imaginal exposures and scripts
When a feared outcome can’t or shouldn’t be tested in real life (e.g., “What if I harmed someone without knowing?”), we write a detailed script of the worst‑case scenario and listen or read repeatedly while practicing response prevention. Imaginal work helps your brain process uncertainty without rituals and prepares you for real‑world moments (6).
Small “everyday” practice between sessions
ERP is a repetition game. We’ll build a doable plan of micro‑exposures—1–5 minute practices that fit daily life (e.g., “touch three ‘iffy’ surfaces before lunch and wait 10 minutes before washing”). Consistency often beats intensity.
🧪 Key takeaway: Many small, consistent reps change your brain faster than one heroic exposure.
Sample ERP Examples by Theme
⚠️ Note: Examples are educational, not prescriptive. Your plan should be tailored to your history, culture, neurotype, and safety.
Contamination and cleaning rituals
Touch a mailbox, then your phone; place the phone in your pocket; wait 30 minutes before washing
Prepare food without re‑washing a “clean” utensil
Sit on your couch after errands in “outside clothes”; notice the urges and let them pass
Therapist moves: Gradually drop covert rituals (e.g., “air‑drying” hands to feel safer, using elbow to open doors) and shift from “How can I make this feel safe?” to “Can I let this be uncertain and do what matters anyway?” (2, 5, 6)
Checking, perfectionism, and “just right” compulsions
Lock the door once, state out loud “Locked once,” leave without photos
Send a message without rereading; if a mistake happens, practice radical acceptance
Place items slightly misaligned and continue your task without fixing
Therapist moves: Add behavioral experiments (e.g., track actual consequences of small imperfections) and practice values‑based actions (e.g., being on time > being perfect) while dropping mental reviews (1, 2, 6)
Harm or scrupulosity obsessions
Carry a small pocketknife at home (if safe/appropriate) while noticing catastrophic thoughts and not seeking reassurance
Walk past a school while labeling thoughts “OCD” and letting them be
Read a self‑written script that begins, “Maybe I am a bad person, and I can’t have 100% certainty,” then move on to a meaningful activity
Therapist moves: Pair exposures with response‑prevention plans for reassurance, confession, or mental neutralizing; emphasize tolerating uncertainty rather than proving innocence (2, 6)
🙏 Key takeaway: ERP for scrupulosity targets certainty‑seeking—not beliefs or values. We respect your faith and work within it.
What ERP Feels Like and How Progress Is Measured
The anxiety curve during exposures
Most people notice a predictable arc: anticipatory anxiety → anxiety peak → gradual drop if you don’t ritualize. The first reps are often the hardest. As your brain updates, the peak shortens and the drop comes sooner. Some sessions feel flat or even more intense—that’s normal. What matters is willingness to practice and follow‑through on response prevention (5, 6).
Signs ERP is working beyond “feeling calm”
You’re spending less time on rituals each day
You do more of what you care about, even with some anxiety present
Urges feel weaker and pass faster
You need less reassurance and can let questions go unanswered
Your Y‑BOCS or other symptom scores improve over weeks (1, 2)
📈 Key takeaway: The goal isn’t zero anxiety; it’s more life with fewer rituals—and evidence shows ERP can get you there (1, 2, 3).
How ScienceWorks Adapts ERP for Neurodivergent Clients
Pacing for ADHD, autism, and sensory needs
Many clients we serve identify as ADHD, autistic, or both. We adjust ERP by:
Using briefer, more frequent reps for attention variability
Building visual plans and external reminders
Tweaking sensory load (e.g., noise, textures) so exposures target OCD—not overwhelm
Offering I‑CBT or combined approaches when a cognitive roadmap helps (see our page on specialized therapy at ScienceWorks)
We can also anchor ERP to skills from executive function coaching—time‑blocking, habit stacking, and reinforcement—to support carry‑through between sessions.
Coordinating ERP with other treatments in Tennessee
ScienceWorks provides secure, HIPAA‑compliant telehealth across Tennessee. We coordinate with prescribers and other therapists when helpful and can add psychological assessments to clarify diagnoses, co‑occurring conditions, or progress over time. If sleep is a sticking point, we integrate CBT‑I for insomnia. You can meet our clinicians on Meet Us and explore current groups. When you’re ready, schedule a free consultation.
🧩 Key takeaway: ERP is not one‑size‑fits‑all. We adapt the plan to your neurotype, culture, and daily realities so practice is doable and sustainable.
Quick FAQ
Is ERP safe? With a trained clinician, ERP is structured and collaborative. We don’t do anything dangerous; we practice uncertainty safely (3, 4).
How long does ERP take? Courses vary. Many clients notice meaningful change in weeks, especially with consistent at‑home practice (1, 2, 6). Individual results vary.
Can ERP be done online? Yes—telehealth ERP is feasible and can be effective, and it’s often ideal for practicing in your actual environment (7, 8, 9).
Next Steps
If you’re looking for OCD treatment in Tennessee or an OCD therapist in Tennessee trained in ERP, we’d love to talk. Learn more about OCD treatment at ScienceWorks or schedule a free consultation to see whether ERP—or an adapted approach—is a fit.
References and Citations
Olatunji, B. O., Davis, M. L., Powers, M. B., & Smits, J. A. J. (2013). Cognitive‑behavioral therapy for obsessive‑compulsive disorder: A meta‑analysis of treatment outcome and moderators. Journal of Psychiatric Research, 47(1), 33–41. https://doi.org/10.1016/j.jpsychires.2012.08.020
Reid, J. E., Laws, K. R., Drummond, L., Vismara, M., Grancini, B., Mpavaenda, D., & Fineberg, N. A. (2021). Cognitive behavioural therapy with exposure and response prevention in the treatment of obsessive‑compulsive disorder: A systematic review and meta‑analysis of RCTs. Comprehensive Psychiatry, 106, 152223. https://doi.org/10.1016/j.comppsych.2021.152223
National Institute for Health and Care Excellence (NICE). (2005, last reviewed 2024). Obsessive‑compulsive disorder and body dysmorphic disorder: Recognition, assessment and treatment (CG31). https://www.nice.org.uk/guidance/cg31
American Psychiatric Association. (2007). Practice guideline for the treatment of patients with obsessive‑compulsive disorder. Arlington, VA: APA. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ocd-1410197738287.pdf
Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. https://doi.org/10.1037/0033-2909.99.1.20
Hezel, D. M., & Simpson, H. B. (2019). Exposure and response prevention for obsessive‑compulsive disorder: A review and new directions. Indian Journal of Psychiatry, 61(Suppl 1), S85–S92. https://pubmed.ncbi.nlm.nih.gov/30745681/
Fletcher, T. L., Boykin, D. M., Helm, A., Dawson, D. B., Ecker, A. H., Freshour, J., … Hundt, N. E. (2021). A pilot open trial of video telehealth‑delivered exposure and response prevention for obsessive‑compulsive disorder in rural veterans. Military Psychology, 34(1), 83–90. https://doi.org/10.1080/08995605.2021.1970983
Voderholzer, U., Meule, A., Koch, S., Pfeuffer, S., Netter, A.‑L., Lehr, D., & Zisler, E.‑M. (2024). Effectiveness of one videoconference‑based exposure and response prevention session at home in adjunction to inpatient treatment in persons with obsessive‑compulsive disorder: Nonrandomized study. JMIR Mental Health, 11, e52790. https://doi.org/10.2196/52790
Wiese, A. D., Kuckertz, J. M., Bamelis, L., & McNally, R. J. (2022). Provider perceptions of telehealth and in‑person exposure and response prevention for obsessive‑compulsive disorder. Psychiatry Research, 313, 114610. https://doi.org/10.1016/j.psychres.2022.114610
This article is for informational and educational purposes only and is not a substitute for diagnosis, medical advice, or treatment. Always consult a qualified professional for your unique situation. Individual results vary.