Pure O & Mental Rituals: What Counts as a Compulsion (Even When It’s “Only in Your Head”)
- Kiesa Kelly

- Dec 21, 2025
- 9 min read
If you live with pure o ocd, you may feel like you’re battling your brain all day long—intrusive thoughts you didn’t ask for, plus an urgent need to do something internally to feel safe again. Because those “somethings” can be silent and subtle, many people wonder: Do I even have compulsions?
In this article, you’ll learn:
Why “Pure O” isn’t actually “no compulsions”
What mental compulsions can look like in real life
How reassurance (including self-reassurance) quietly keeps OCD stuck
How ERP for mental compulsions works when rituals happen in your head
What to ask an OCD therapist if you’re seeking help in Tennessee
Key takeaway: 🧠 If a thought triggers urgency and you respond with a ritual to feel certain or “safe,” that response may be a compulsion—even if it’s invisible.
Pure O isn’t “no compulsions” — it’s often invisible compulsions
Why the term “Pure O” is misleading (and why it still feels real)
“Pure O” is commonly used to describe OCD that seems dominated by obsessions—intrusive thoughts, images, or urges—without obvious outward rituals. The problem is that OCD rarely stops at obsessions.
Compulsions can be mental acts (like praying, repeating phrases silently, or “reviewing” memories) or behaviors that blend into daily life (like avoidance and reassurance-seeking). In other words: it’s not “purely obsessions”—it’s often compulsions you can’t see.[1–3]
Here are three common misconceptions that keep people stuck:
Misconception #1: “If I’m not washing or checking, it’s not OCD.” (Mental rituals count.)[1–3]
Misconception #2: “If I can’t stop thinking, that means I need to solve it.” (Rumination is often the compulsion.)[4,5]
Misconception #3: “Reassurance is healthy because it calms me down.” (Short-term relief can reinforce long-term fear.)[6]
Compulsions can be mental, subtle, and constant
Clinically, compulsions include repetitive behaviors or mental acts done to reduce distress or prevent a feared outcome.[1,2] In “Pure O,” the compulsion is often a private
strategy: trying to get certainty, trying to feel “right,” or trying to make the thought go away.
Key takeaway: 🔎 A compulsion isn’t defined by how visible it is—it’s defined by its function: reducing distress and chasing certainty.
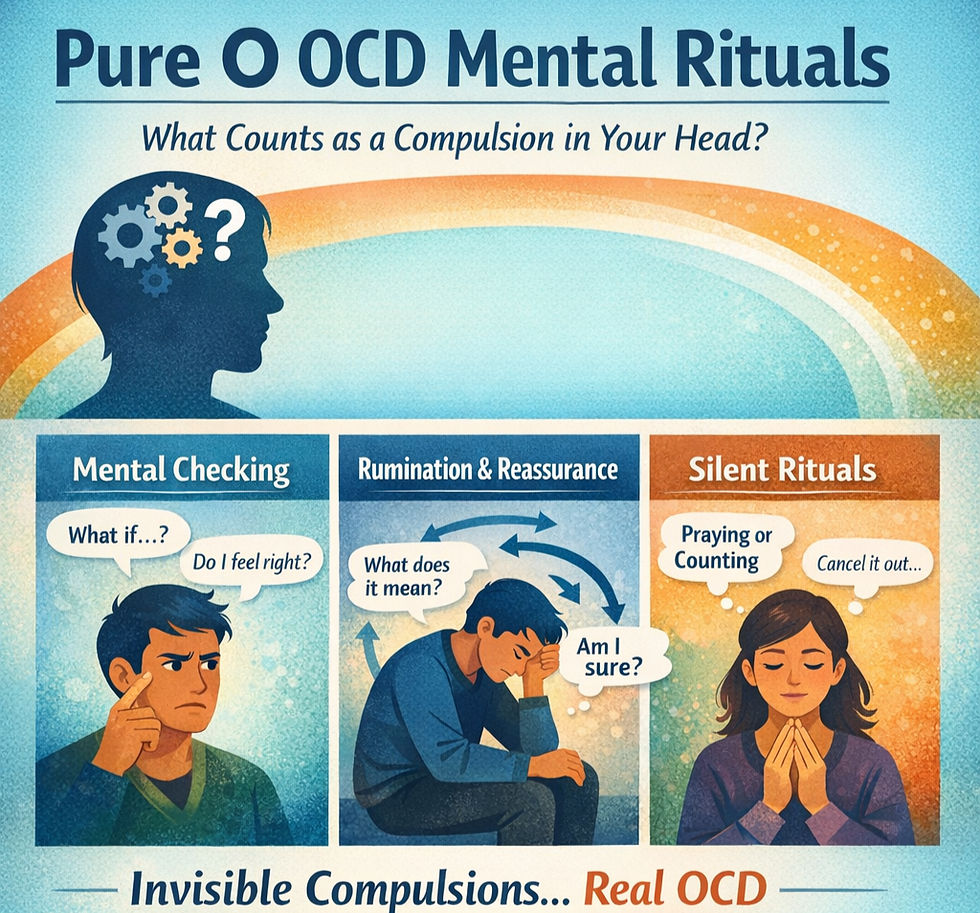
What counts as a mental compulsion (with real-life examples)
Mental compulsions can be hard to spot because they can feel like “just thinking.” A helpful rule of thumb: Does the thinking feel urgent, repetitive, and aimed at getting relief or certainty? If yes, it may be a compulsion.[4,5]
Mental checking: “Do I feel anxious? Did I mean it? What if…?”
Mental checking is internal monitoring to prove something is (or isn’t) true.
Examples:
Re-reading your own intentions: “Did I actually mean that?”
Checking your emotional response: “Do I feel guilty enough?”
Checking your body: “Was that arousal… or just a random sensation?”
Checking memory: replaying a moment to confirm you didn’t “mess up”
This is especially common in OCD intrusive thoughts that latch onto identity, morality, relationships, or harm. The checking is an attempt to get certainty—something OCD never truly allows.
Neutralizing: replacing thoughts, praying “until it feels right,” canceling thoughts
Neutralizing is an internal “undo.” It can look like:
Saying a phrase in your head to cancel a thought
Praying or repeating a mantra until the anxiety drops
Replacing “bad” images with “good” images
Mentally “confessing” or apologizing to feel clean again
These are mental rituals: repeated, rule-bound actions meant to reduce distress.[1–3]
Rumination/problem-solving loops disguised as “figuring it out”
Rumination is one of the sneakiest compulsions because it feels responsible:
“I need to understand what this thought means about me.”
“If I can find the perfect explanation, I’ll stop spiraling.”
“Let me run through every possibility—just in case.”
But in OCD, rumination is often a loop that keeps you fused to doubt rather than living your life. IOCDF clinicians describe rumination as a form of compulsion when it’s goal-directed toward relief and certainty.[4,5]
Key takeaway: 🔁 If the “figuring it out” never actually finishes—because OCD moves the goalposts—that’s a clue it’s a compulsion.
The reassurance cycle — why it works short-term and backfires long-term
Relief teaches the brain the thought was dangerous
Reassurance (from others or yourself) can feel like oxygen. You ask, you get a soothing answer, your anxiety drops. The brain learns: “That thought was a threat, and reassurance saved me.” Over time, that learning makes the next intrusive thought feel even more urgent.[2,6]
Research on reassurance seeking supports its role as a maintaining factor in anxiety and OCD patterns.[6]
How reassurance morphs into self-reassurance (internal debates, “reviewing”)
In pure o ocd, reassurance often turns inward:
Debating with yourself like a lawyer
Reviewing “evidence” for and against the fear
Replaying a memory to prove you’re safe
Telling yourself “I would never do that” repeatedly
It’s still reassurance—it’s just happening silently.
Key takeaway: 🧯 Reassurance reduces distress now, but it usually increases doubt later—because your brain never learns you can handle uncertainty.
Mental rituals you might not recognize as compulsions
“Researching to feel certain” (Googling, forums, checking definitions)
If you’ve ever fallen into hours of searching—symptoms, definitions, “does anyone else…,” moral debates—that may be a compulsion. The goal is usually certainty: “If I can just know for sure, I’ll be okay.”
This can also look like:
Reading the same article repeatedly
Comparing yourself to other people’s stories
Looking for the “right” label to make the fear go away
Body scanning and emotion checking (love, attraction, guilt, arousal, “rightness”)
Many people with Pure O don’t just fear the thought—they fear what their body or emotions might “reveal.”
So the compulsion becomes scanning:
“Do I feel love right now?”
“Am I attracted… or not?”
“Do I feel enough guilt to prove I’m a good person?”
“Does my body feel ‘right’?”
This constant monitoring can make feelings less clear over time, because anxiety changes sensation.
Avoidance that looks like “being responsible” (dodging triggers, people, topics)
Avoidance can be physical or mental:
Avoiding content, people, or situations that trigger uncertainty
Avoiding certain words or topics “just in case”
Avoiding decisions because you want perfect certainty first
Avoidance is understandable—but it also teaches the brain that triggers are dangerous.
Key takeaway: 🧭 If your day is organized around preventing triggers or checking your inner state, OCD may be running the schedule.
If it’s “just a thought,” why does it feel so urgent?
Intrusive thoughts are common; OCD is the relationship to the thought
Most humans have unwanted, weird, or disturbing thoughts. Classic research found that intrusive thoughts can occur in both clinical and non-clinical populations; what differs is how the thoughts are interpreted and responded to.[7]
In OCD, the thought lands like a threat. The mind tries to neutralize it, prove it wrong, or get certainty. That reaction—especially compulsive rituals—keeps the thought sticky.[5,7]
If you’re searching for how to deal with OCD intrusive thoughts, the surprising answer is often: less arguing with the thought, more changing your response to it.
Why shame and secrecy make Pure O louder (and more isolating)
Pure O themes often involve taboo topics (harm, sexuality, religion, morality). Shame can lead people to hide symptoms, which makes OCD more powerful: you feel alone, you don’t reality-check with a clinician, and the mind treats the thought as even more dangerous. It’s common—and treatable.[4,5]
Key takeaway: 🌿 Having an intrusive thought is not a character test. OCD is the disorder of “what if,” not the disorder of who you are.
What evidence-based treatment looks like for Pure O
ERP for mental rituals: focusing on response prevention (not perfect exposures)
ERP (Exposure and Response Prevention) is a frontline, evidence-based treatment for OCD.[3,8,9] For Pure O, the “exposure” may include approaching triggers (images, situations, uncertainty) and the “response prevention” is often the bigger lift: not doing the mental ritual.[3,8]
A practical example (not a script):
Trigger: an intrusive doubt pops up.
Old response: immediate analysis, checking feelings, and self-reassurance.
ERP response prevention: noticing the urge, labeling it (“that’s reassurance-seeking”), and choosing not to engage—returning attention to your values-based activity.
This is why many people benefit from working with an OCD therapist: you learn to identify rituals, build a plan, and practice gradually.
Key takeaway: 🧱 ERP for pure o isn’t about forcing scary thoughts—it’s about preventing the rituals that keep the thoughts powerful.
I-CBT and doubt-based OCD: stepping out of the “maybe” story
Inference-Based CBT (I-CBT) is another evidence-based approach that targets OCD’s “doubt story”—the shift from reality-based information to a hypothetical narrative (“Maybe… what if… it could mean…”).[10,11] Research on inference-based approaches shows promising outcomes, including for people who struggle with insight or who feel trapped in mental rituals.[10,11]
In practice, I-CBT helps you:
Identify the moment you leave reality and enter the “maybe” world
Notice the reasoning errors that keep doubt believable
Reconnect with real-world information and lived experience
Many clinicians integrate ERP and I-CBT, especially when OCD is heavily cognitive or when compulsions are primarily mental.
Safety note: why you don’t have to DIY high-stakes exposures alone
Some exposures (or feared scenarios) touch on safety, legal, ethical, or trauma-related boundaries. You don’t need to “prove” anything by taking risky steps. Evidence-based OCD treatment is structured, collaborative, and designed to keep you safe while reducing avoidance and ritualizing.[8]
Getting help (and what to ask an OCD specialist)
If you’re looking for an OCD therapist—especially if you’ve been told you have “only intrusive thoughts”—it’s reasonable to ask directly about experience with mental rituals.
Questions to ask: ERP experience, I-CBT training, handling mental compulsions
Consider asking:
“How do you identify and treat mental compulsions like rumination and reassurance?”
“Do you provide erp therapy for pure o / erp for mental compulsions specifically?”
“Are you trained in I-CBT or other cognitive approaches for doubt-based OCD?”
“How do you handle safety and boundaries for taboo themes without doing reassurance?”
Telehealth in Tennessee: what can be done online and what progress looks like
Many people make meaningful progress in OCD treatment through telehealth, particularly when therapy is structured and skills-based.[12] If you’re searching for ocd therapists in tennessee, you can ask whether the clinician offers remote ERP sessions, between-session support structures, and clear ways to track progress (like reduced rituals and increased flexibility—not “perfect certainty”).
At ScienceWorks Behavioral Healthcare, we offer specialized, evidence-based care for OCD, including ERP and I-CBT, and we work to make treatment practical for real life.
You can explore our services here:
Learn about our OCD therapy services: OCD treatment at ScienceWorks
See our approach to specialized care: Specialized therapy options
Meet our clinicians: Meet the ScienceWorks team
Ask about groups and skills practice: Groups at ScienceWorks
If you’re also considering assessment: Psychological assessments
Ready to take the next step: Contact
Next steps
If this article helped you recognize mental rituals you hadn’t named before, you’re not alone—and you’re not “making it up.” Pure O can be exhausting precisely because the compulsions look like thinking. With the right framework, you can learn to notice the loop, reduce rituals, and get your life back—without having to win an argument with your brain.
If you’d like support from an OCD specialist, consider reaching out for a consultation to talk through your symptoms, treatment options (ERP, I-CBT, or both), and what care could look like through telehealth in Tennessee.
About the Author
Dr. Kiesa Kelly is the owner and psychologist at ScienceWorks Behavioral Healthcare. She earned her PhD in Clinical Psychology with a concentration in Neuropsychology from Rosalind Franklin University of Medicine and Science and completed extensive clinical training across university and medical settings, including an NIH-funded postdoctoral fellowship at Vanderbilt University.
At ScienceWorks, Dr. Kelly provides specialized therapy for OCD and related concerns using evidence-based approaches such as Exposure and Response Prevention (ERP) and Inference-Based CBT (I-CBT), with an emphasis on compassionate, neurodivergent-affirming care.
References
American Psychiatric Association. What is obsessive-compulsive disorder? American Psychiatric Association; n.d.
National Center for Biotechnology Information. DSM-IV to DSM-5 Obsessive-Compulsive Disorder criteria table (compulsions include mental acts). NCBI Bookshelf; n.d.
National Institute for Health and Care Excellence (NICE). Obsessive-compulsive disorder and body dysmorphic disorder: treatment (CG31). London: NICE; 2005 (updated).
International OCD Foundation. How do I stop thinking about this? What to do when you’re stuck playing mental ping-pong. IOCDF; n.d.
International OCD Foundation. Ruminating on ruminations: mental compulsions and what to do about them. IOCDF; 2023.
Rector NA, et al. Reassurance seeking in the anxiety disorders and OCD. J Anxiety Disord. 2019; DOI: https://doi.org/10.1016/j.janxdis.2019.102109.
Rachman S, de Silva P. Abnormal and normal obsessions. Behav Res Ther. 1978;16(4):233–248. DOI: https://doi.org/10.1016/0005-7967(78)90022-0.
International OCD Foundation. Exposure and response prevention (ERP). IOCDF; n.d.
Koran LM, et al. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007;164(7 Suppl):5–53.
O’Connor KP, et al. Evaluation of an inference-based approach to treating obsessive-compulsive disorder. Cogn Behav Ther. 2005;34(3):148–163. DOI: https://doi.org/10.1080/16506070510041211.
Williams MT, Farris SG, Turkheimer E, et al. Myth of the pure obsessional type in obsessive-compulsive disorder. Depress Anxiety. 2011;28(6):495–500. DOI: https://doi.org/10.1002/da.20820.
Lundström L, Flygare O, Andersson E, et al. Effect of internet-based vs face-to-face cognitive behavioral therapy for adults with obsessive-compulsive disorder: a randomized clinical trial. JAMA Netw Open. 2022;5(3):e221967. DOI: https://doi.org/10.1001/jamanetworkopen.2022.1967.
Final disclaimer: This article is for informational purposes only and is not a substitute for professional diagnosis, treatment, or medical advice.