I-CBT for OCD: How Inference Based Therapy Works (and When It Helps)
- Ryan Burns

- Oct 12, 2025
- 5 min read

When you’re living with OCD, it can feel like your brain is constantly asking, “But what if…?” Inference-Based Cognitive Behavioral Therapy (I-CBT) was designed specifically for that experience. Instead of leaning primarily on prolonged exposure exercises, I-CBT teaches you to recognize how OCD reasons you into doubt, then replace those imagined possibilities with present-moment evidence and values-guided action. In this guide, you’ll learn what I-CBT is, how it works, when it helps, and how we use it at ScienceWorks to support lasting change. (1)(2)(3)
What is I-CBT?
I-CBT targets the reasoning glitches that create obsessional doubt—what researchers call inferential confusion. Rather than arguing with content (e.g., “Did I contaminate someone?”), you learn to spot the moment your mind leaves reality for an imagined possibility and to come back to direct evidence. Several clinical trials and reviews indicate I-CBT is an effective, evidence-based treatment for OCD. (1)(3)(4)
How I-CBT Works: From Imagined Possibility to Present Evidence
I-CBT typically follows a clear, collaborative progression:
Map the OCD story – Identify triggers and the narrative that pulls you from perception into “maybe” thinking.
Spot inferential confusion – Notice the shift from real-world cues to remote possibilities, stereotypes, or feared-self themes.
Re-anchor in reality – Check sensory information and credible context; rebuild trust in present-moment evidence.
Choose values-aligned actions – Reduce checking/mental rituals and re-engage with what matters.
Practice skills between sessions – Brief, targeted exercises that generalize to daily life.
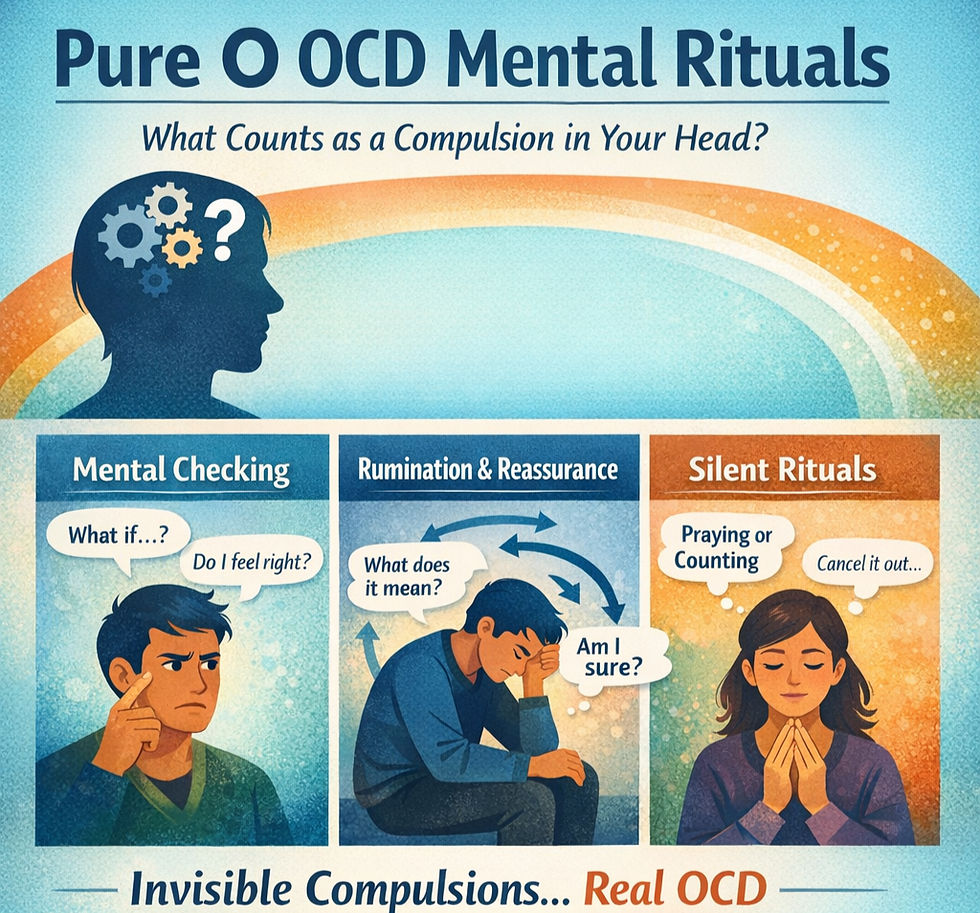
Across open trials and randomized studies, this cognitive pathway has produced meaningful reductions in OCD severity and appears particularly helpful for people with high overvalued ideas or “pure-O” presentations dominated by intrusive thoughts and mental rituals. (1)(3)(4)
I-CBT for OCD vs. ERP: What’s the difference?
ERP (Exposure and Response Prevention) is the first-line psychotherapeutic treatment for OCD overall, with strong evidence across decades. It relies on approaching feared cues without rituals. (5)(6)
I-CBT is a cognitive route that reduces reliance on deliberate exposure by correcting obsessional reasoning. Recent large trials suggest I-CBT performs about as well as standard CBT packages, with indications of better tolerability for some people (e.g., fewer dropouts or higher acceptability) even though non-inferiority to CBT with ERP was statistically inconclusive in one multisite trial. (1)(2)
Bottom line: If ERP feels too threatening right now—or you mainly struggle with intrusive thoughts and mental rituals—I-CBT can be a solid, evidence-based alternative or complement. Individual results vary. (1)(2)(5)
Who is I-CBT for OCD best for?
People who often benefit from I-CBT include those who:- Experience primarily mental compulsions (rumination, reassurance seeking, reviewing).- Hold strong overvalued ideas or feared-self themes (e.g., “What if I’m secretly dangerous/immoral?”).- Feel overwhelmed by exposure work or prefer a gentler entry point.- Are neurodivergent and respond better to structured reasoning tools and stepwise skill-building. (1)(4)
If you’re unsure which path fits, we can help you decide in a free consultation and, when helpful, begin with a psychological assessment to clarify diagnosis and tailor the plan.
What treatment with ScienceWorks looks like
At ScienceWorks Behavioral Healthcare, our care is science-informed, warm, and collaborative. Depending on your goals, your plan may include:
I-CBT as a primary approach when obsessional doubt and mental compulsions dominate.
ERP elements when exposure accelerates progress on specific triggers. (5)(6)
ACT-style skills (values, willingness) to support behavior change.
Coaching supports (e.g., Executive Function Coaching) for planning, accountability, and skill carryover.
Measurement-based care with regular symptom tracking to guide decisions.
Integrated services, including specialized therapy, assessment, OCD care, and therapy groups.
Want to meet us first? Explore our team and book a consultation.
Evidence check: Does I-CBT really work?
A 2022 multicenter RCT found I-CBT and mindfulness-based stress reduction produced outcomes comparable to standard “appraisal-based” CBT, with signals that I-CBT may remit symptoms faster and be especially helpful for overvalued ideas. (1)
A 2024 multisite non-inferiority RCT comparing I-CBT directly to CBT (with ERP) reported no conclusive non-inferiority on the primary outcome, yet higher tolerability for I-CBT—useful for people who struggle to engage with exposure. (2)
Earlier trials and comprehensive reviews support I-CBT/IBA mechanisms and effectiveness across OCD subtypes. (3)(4)
ERP remains a first-line treatment with robust meta-analytic support; many clients benefit from both approaches, selected based on fit and goals. (5)(6)
FAQs
Is I-CBT “exposure-free”?
I-CBT does not require prolonged, formal exposure sessions. You’ll still practice real-life actions (e.g., reduce checking) as your confidence in reality-based reasoning grows. (1)(4)
How many sessions will I need?
Many I-CBT protocols run ~18–24 sessions. Your plan is individualized, paced by readiness, symptom pattern, and progress metrics. (1)(3)
Will I-CBT work if ERP hasn’t helped?
Possibly. I-CBT can be a good option if ERP felt intolerable, you mainly have intrusive thoughts/mental rituals, or you hold strong overvalued ideas. We’ll help you choose—and we can blend approaches. (1)(2)(5)
What to do next
If this sounds like the right fit, request an assessment or schedule a free consultation to start I-CBT for OCD via secure telehealth. Learn more about OCD care at ScienceWorks.
References
1. Aardema, F., Bouchard, S., Koszycki, D., Lavoie, M.-E., Audet, J.-S., & O’Connor, K. (2022). Evaluation of Inference-Based Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder: A Multicenter Randomized Controlled Trial with Three Treatment Modalities. Psychotherapy and Psychosomatics, 91(5), 348–359. https://doi.org/10.1159/000524425
2. Wolf, N., van Oppen, P., van Megen, H., et al. (2024). Inference-Based Cognitive Behavioral Therapy versus Cognitive Behavioral Therapy for Obsessive-Compulsive Disorder: A Multisite Randomized Controlled Non-Inferiority Trial. Psychotherapy and Psychosomatics, 93(6), 397–411. https://doi.org/10.1159/000541508
3. O’Connor, K. P., Aardema, F., Bouthillier, D., Fournier, S., Guay, S., Robillard, S., … Pitre, D. (2005). Evaluation of an Inference-Based Approach to Treating Obsessive-Compulsive Disorder. Cognitive Behaviour Therapy, 34(3), 148–163. https://doi.org/10.1080/16506070510051532
4. Julien, D., O’Connor, K. P., & Aardema, F. (2016). The inference-based approach to obsessive-compulsive disorder: A comprehensive review of its etiological model, treatment efficacy, and model of change. Journal of Affective Disorders, 202, 187–196. https://doi.org/10.1016/j.jad.2016.05.060
5. Song, M., Kim, B., & Park, S. (2022). Effectiveness of exposure and response prevention in the treatment of obsessive–compulsive disorder: A meta-analysis. Psychiatry Research, 317, 114861. https://doi.org/10.1016/j.psychres.2022.114861
6. McKay, D., Sookman, D., Neziroglu, F., Wilhelm, S., Stein, D. J., Kyrios, M., Matthews, K., & Veale, D. (2015). Efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Psychiatry Research, 225(3), 236–246. https://doi.org/10.1016/j.psychres.2014.11.058
Disclaimer
This content is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, licensed psychologist, or other qualified health provider with any questions you may have regarding a medical or mental health condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.