What “Evidence-Based” Looks Like in a Real Therapy Practice: Evidence-Based Therapy Practice Culture
- Ryan Burns

- 2 days ago
- 7 min read
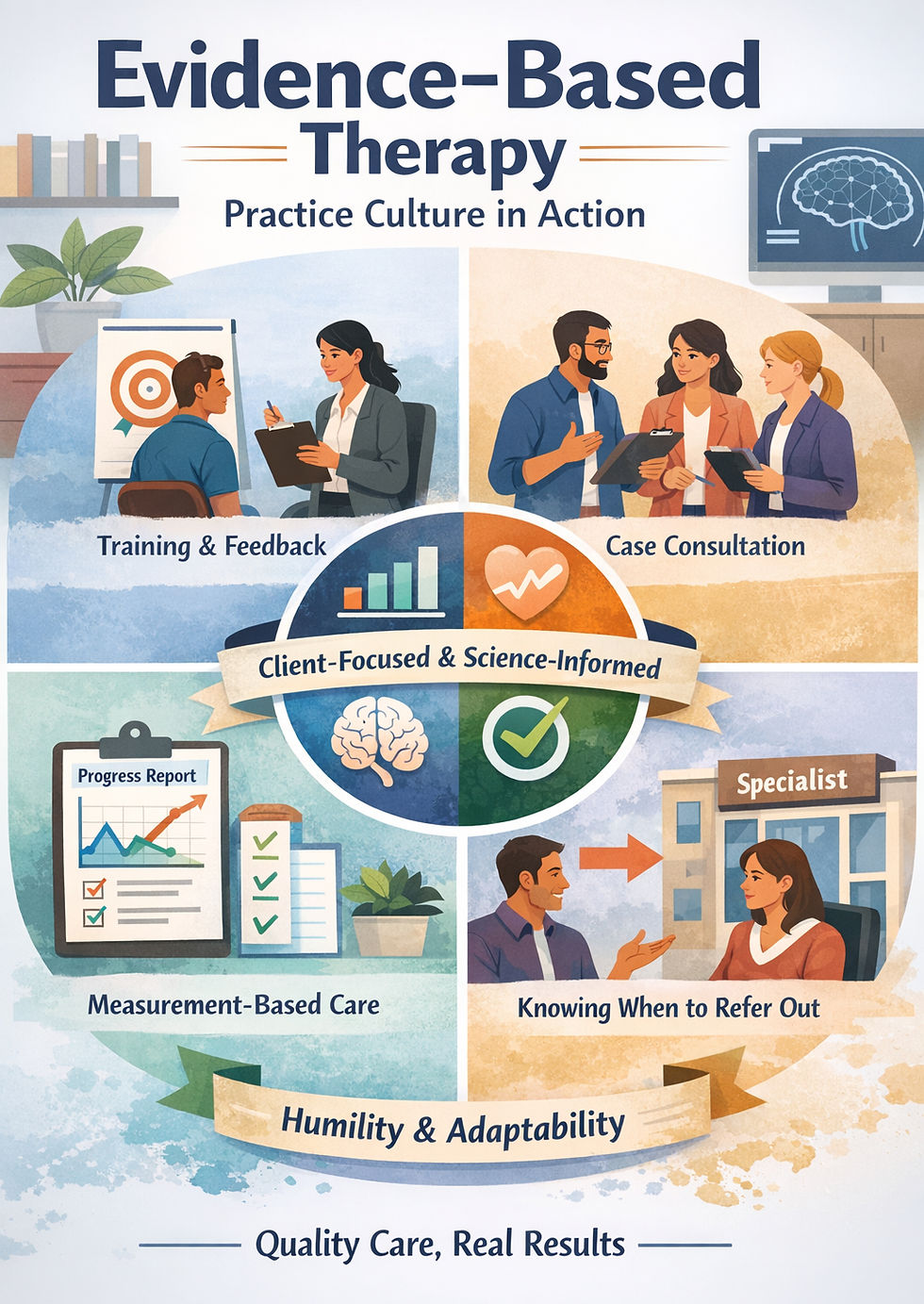
When we talk about evidence-based therapy practice culture, we’re not talking about a perfect therapist who always “gets it right.” We’re talking about a practice environment that makes good clinical thinking easier to do consistently: clear goals, ongoing feedback, case consultation, and the humility to change course when something isn’t helping. The APA’s evidence-based practice framework emphasizes integrating the best available research with clinical expertise, in the context of client characteristics, culture, and preferences. [1]
In this article, you’ll learn:
How “Evidence-based” gets misused (and what it is not)
The three ingredients that make care truly evidence-informed
What evidence-based habits look like in day-to-day sessions
How consultation and training protect both clients and clinicians
Why humility (scope, culture, outcomes) is part of the evidence
💡 Key takeaway: “Evidence-based” isn’t a marketing label. It’s a set of daily behaviors that keep care aligned with both science and the client’s reality. [1]
Why “Evidence-Based” Gets Misused
“Evidence-based” should be a quality signal. But in mental health, it sometimes turns into a vague promise that means very little.
Evidence-based ≠ rigid scripts
Structured approaches (manuals, protocols, stepwise models) can be part of evidence-based care—especially when a concern has strong research support for specific methods. But structure isn’t the same thing as rigidity. Evidence-based care uses evidence as a map, then adapts the route based on the person in the room. [1]
Evidence-based ≠ “whatever is trendy on social media”
Some ideas trend because they’re validating or easy to share. That doesn’t make them wrong, but it does mean they need context and humility. A practice can be warm, trauma-informed, and culturally responsive without letting trends replace formulation, ethics, or outcomes tracking.
Evidence-based ≠ “the relationship doesn’t matter”
Evidence-based practice explicitly includes clinician expertise and client factors, which means the relationship, fit, and context matter. [1] The most “correct” intervention won’t help much if a client feels judged, rushed, or misunderstood.
The Three-Leg Stool of Evidence-Based Care
A practical way to remember evidence-based practice is a “three-leg stool”:
Research evidence (what we know)
Research helps us choose methods with the best odds of helping, anticipate risks, and sequence care. In other words: we don’t ignore what the field has learned. [1]
Clinical expertise (pattern recognition + skill)
Research doesn’t walk into your office; people do. Clinical expertise is the ability to apply evidence well: formulation, pacing, communication, and skilled delivery—especially with comorbidity and real-world constraints.
Client values (autonomy and fit)
Evidence-based care is collaborative. It requires shared decision-making about goals, tradeoffs, and what “better” means to the client. [2]
💡 Key takeaway: If any leg is missing—research, expertise, or client values—care gets wobbly fast. [1]
What This Looks Like Day to Day
Here’s what evidence-based habits look like in real schedules, not just in training slides.
Clear case conceptualization and shared goals
A strong practice culture supports clinicians in answering, early and often:
What’s maintaining the problem?
What are we targeting first?
How will we know therapy is working?
Example: A client with OCD wants “certainty” that they’re safe and “not a bad person.” A clear plan reframes the goal: reducing compulsions, increasing uncertainty tolerance, and reconnecting with values. If you want to see what structured OCD care can look like, here’s our overview of ERP therapy for OCD in Nashville. [11]
Ongoing reflection: “Is this helping?”
Evidence-based teams don’t rely on vibes alone—they check.
Measurement-based care (MBC) is one common way to do this: brief, routine measures used to monitor progress and inform decisions. [3] The point isn’t to turn therapy into a spreadsheet; it’s to notice early when progress stalls.
Example: An OCD client completes a weekly severity check-in (like the Y-BOCS OCD severity tracker) and sees that distress is dropping, but avoidance isn’t. That data can guide the next step: shifting from insight work to more in-session exposures, or tightening the response-prevention plan. [10]
Adjusting course without blaming the client
When something isn’t working, evidence-based care changes the plan—without turning the problem into “client resistance.”
Example: A neurodivergent adult in burnout can understand tools perfectly but still can’t implement them. The adjustment might be reducing cognitive load, making goals smaller, and choosing one measurable “capacity metric” (sleep, recovery time, sensory breaks) instead of adding more homework. MBC supports this by showing whether changes are helping. [3]
💡 Key takeaway: Progress tracking isn’t about grading clients. It’s about making sure the plan still fits—and changing it when it doesn’t. [3]
Consultation as a Culture in an Evidence-Based Therapy Practice Culture
In many settings, consultation only happens when a clinician feels overwhelmed. In a healthier culture, it’s routine.
How consult prevents stuckness and clinician isolation
Isolation is a quiet driver of clinical drift. Consultation helps clinicians regain perspective, test alternative formulations, and spot ethical or scope concerns early—before a “stuck case” becomes a morale problem.
The difference between consultation and supervision
When people compare clinical supervision vs consultation, the difference is usually structure and responsibility.
Clinical supervision is typically formal and evaluative, focused on developing competence and protecting client welfare (often within training or licensure contexts). [6]Case consultation is typically collaborative and case-focused: a clinician seeks colleague input to improve care while retaining primary responsibility for decisions. [6]
Psychological safety: asking for help without judgment
Consult culture depends on tone: curious, non-shaming, and learning-oriented. It sounds like: “Here’s what I tried. Here’s where I’m unsure. What am I missing?” That psychological safety protects clients because it keeps clinicians open to feedback.
💡 Key takeaway: Consultation makes humility actionable. It turns uncertainty into learning instead of isolation. [6]
Training That Supports Real Competence
Evidence-based culture doesn’t happen because someone attended a CE once. It happens because a practice invests in skills, feedback, and ongoing development.
ScienceWorks describes “paid training opportunities” as part of its model—what many clinicians would call a paid training therapist pathway—along with internal case consultations on a collaborative clinical team. [8]
Skill-building, not just CE certificates
CE is useful, but real competence shows up in performance: can you deliver the skill, adapt it, and explain it to a client clearly? If a practice claims to be evidence-based, a fair question is whether there’s continuing education support and an expectation of skill demonstration.
Role-plays, feedback, and deliberate practice
Skill grows faster when training includes behavioral rehearsal (role-plays), specific feedback, and repeat practice on the hard parts. That’s how “I know the model” becomes “I can use the model well.”
Specialized pathways for niche work (when relevant)
Some work requires deeper specialization (e.g., OCD treatment fidelity, neurodivergent-affirming assessment, complex trauma). A quality practice helps clinicians know what training is needed, when to consult, and when referral-out is best.
To see how our team describes its approach and specialties, you can meet the ScienceWorks team and explore our specialized therapy services. [9,12]
💡 Key takeaway: Training that changes outcomes usually includes feedback and practice—not just information. [8]
Humility and Ethics Are Part of “Evidence-Based”
Evidence-based practice isn’t only about what works. It’s also about what’s responsible, respectful, and honest.
Scope of practice and referral-out as strength
Ethics guidance emphasizes working within the boundaries of competence, and using training, supervision, consultation, and referral appropriately when needs are outside a clinician’s competence. [4] Sometimes the best evidence-based move is a referral to a different level of care or specialty.
Cultural humility and neurotype-affirming care
Cultural humility is a stance of lifelong self-reflection and attention to power imbalances, not a checklist you can “complete.” [5]
For many clients, that includes neurotype. Neuro-affirmative practice emphasizes inclusive, strengths-aware care that respects individual needs and preferences. [7] Evidence-based culture holds both: validated methods and goals that protect dignity and autonomy.
Avoiding overpromising outcomes
Evidence-based language avoids guarantees. It sounds like: “This approach is supported by research,” and “We’ll track progress and adjust if it isn’t helping.” That honesty protects the relationship and keeps care ethically grounded.
💡 Key takeaway: Evidence-based care includes the humility to say “I don’t know yet,” and the ethics to build a plan that is honest and safe. [4]
If you want a collaborative, evidence-informed team culture
If you’re a clinician who values clear formulation, therapist case consultation, and real skills practice - not just productivity pressure - team culture matters as much as modality.
Sound like the environment you’re looking for? connect with us through our Careers page. [8]
💡 Key takeaway: The best evidence-based culture is collaborative: it supports clinicians so clients get steadier, higher-quality care. [8]
About ScienceWorks
ScienceWorks Behavioral Healthcare is a psychologist-led telehealth practice that emphasizes evidence-informed care, ongoing training, and internal case consultation as part of a collaborative clinical team. [8,9]
References
APA Presidential Task Force on Evidence-Based Practice. Evidence-based practice in psychology. Am Psychol. 2006;61(4):271-285. doi: https://doi.org/10.1037/0003-066X.61.4.271
Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71-72. doi: https://doi.org/10.1136/bmj.312.7023.71
Lewis CC, Boyd MR, Puspitasari A, et al. Implementing Measurement-Based Care in Behavioral Health: A Review. JAMA Psychiatry. 2019;76(3):324-335. doi: https://doi.org/10.1001/jamapsychiatry.2018.3329
American Psychological Association. Ethical principles of psychologists and code of conduct (effective 2003; amended 2010). Washington (DC): DC Health; [cited 2026 Feb 2]. Available from: https://dchealth.dc.gov/sites/default/files/dc/sites/doh/publication/attachments/ETHICAL%20PRINCIPLES%20OF%20PSYCHOLOGISTS%20and%20CODE%20OF%20CONDUCT.pdf
Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117-125. doi: https://doi.org/10.1353/hpu.2010.0233
American Psychological Association. Guidelines for clinical supervision in health service psychology. Am Psychol. 2015;70(1):33-46. doi: https://doi.org/10.1037/a0038112
National Autistic Society. Embracing neurodiversity affirmative practice: a path to better outcomes. National Autistic Society; 2025 Aug 11 [cited 2026 Feb 2]. Available from: https://www.autism.org.uk/advice-and-guidance/professional-practice/embracing-neurodiversity-affirmative-practice
ScienceWorks Behavioral Healthcare. Exciting career opportunities at ScienceWorks. ScienceWorks; [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/careers
ScienceWorks Behavioral Healthcare. Meet the ScienceWorks team. ScienceWorks; [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/meet-us-1
ScienceWorks Behavioral Healthcare. Y-BOCS: Understanding OCD with ScienceWorks. ScienceWorks; 2026 Jan 7 [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/y-bocs
ScienceWorks Behavioral Healthcare. ERP therapy in Nashville for OCD. ScienceWorks; 2025 Dec 18 [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/info/erp-therapy-in-nashville-for-ocd
ScienceWorks Behavioral Healthcare. ScienceWorks: Trusted Mental Health Therapy & Support (Specialized Therapy). ScienceWorks; [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/specialized-therapy
ScienceWorks Behavioral Healthcare. Medical trauma: an overlooked aspect of chronic illness (About the Author). ScienceWorks; 2025 May 2 [cited 2026 Feb 2]. Available from: https://www.scienceworkshealth.com/post/medical-trauma-an-overlooked-aspect-of-chronic-illness
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical, psychological, or legal advice, diagnosis, or treatment.



