From Solo to Group Practice: What Changes When You Start hiring
- Ryan Burns

- 2 days ago
- 6 min read

If you’re Googling how to start a group practice, you’re likely feeling two things at once: relief that demand is steady, and worry that hiring will make everything messier. Both can be true. Growing from solo to team is less about “adding clinicians” and more about building a reliable way of working together so hiring therapists for group practice doesn’t turn into chaos.
In this article, you’ll learn:
The leadership shift that surprises most solo owners
When it’s actually time to hire (and when it’s not)
The minimum systems you need before onboarding therapists
How compensation models shape expectations and culture
How to keep clinical standards high as you scale
When a “platform” model might fit better than DIY growth
The First Big Shift: You’re Building a Business and a Team
Why “more clinicians” isn’t automatically “more freedom”
One clinician can expand access fast. It can also add recruiting, onboarding, supervision, quality checks, and “people problems” you didn’t have when it was just you.
🧭 Key takeaway: Hiring buys capacity, not simplicity. Plan for leadership time to be part of the job.
Practical example: A solo practice with a six-week waitlist hires one therapist. Referrals spike, but intake questions pile up, notes look inconsistent, and clients get mixed messages about cancellations. The fix isn’t “work harder” - it’s clearer systems.
The new work: leadership, systems, and consistency
A strong therapist-owner “systems” mindset (think: group practice systems therapist) is less “do it my way” and more “make the right way easy.” This is leadership for therapists in real time. Expect to spend time on:
Shared clinical expectations (scope, consultation, referral thresholds)
Repeatable workflows (intake, notes, billing, follow-up)
Feedback loops (so small issues get repaired quickly)
Culture (so the tone stays shame-reducing, not punitive)
When It’s Time: How to Start a Group Practice Counseling With Your First Hire
You have stable demand and predictable operations
Look for patterns over time:
Referrals come from a few reliable sources
Your intake process works even when you’re busy
Your schedule is full with a predictable cancellation rate
Misconception #1: “I’ll hire to fix my marketing.” Group practice marketing is easier when operations can already handle more volume.
📈 Key takeaway: Hire when demand is steady and your intake can handle growth without heroics.
Your own caseload is steady enough to support leadership time
If you stay maxed out clinically, leadership gets shoved into nights and weekends, and resentment builds. Before hiring, create space for interviews, onboarding, consultation, and fixing workflow snags.
Misconception #2: “I can keep my full caseload and lead a team after hours.” Most owners eventually reduce sessions to lead well.
You can define “what good looks like” clinically and operationally
Before you onboard therapists, write down your baseline standards:
Clinically: scope boundaries, consultation triggers, referral thresholds
Operationally: note timelines, messaging expectations, cancellation handling
✅ Key takeaway: If you can’t describe “what good looks like,” you can’t hire for it or coach to it.
The Infrastructure You Need Before Hiring
Policies, procedures, and documentation standards
Practice policies and procedures reduce ambiguity. Start with informed consent and privacy practices, attendance/cancellation, documentation standards (format + timing), and after-hours boundaries.
If you’re starting a group practice in Tennessee, double-check discipline-specific board rules on documentation and record retention. For example, Tennessee psychology rules include minimum retention timeframes. [4]
Scheduling/billing workflows (and who owns what)
Clarify, in writing:
Who schedules (client, clinician, admin)?
Who owns benefit checks, claims, and follow-up?
How are late cancels/no-shows handled?
How and when do clinicians get paid?
Practical example: If clinicians are expected to verify benefits but don’t have training or portal access, the workflow collapses. Assign “ownership” to roles, not personalities.
Risk management basics (without legal deep-dives)
Keep the basics consistent:
Minimum-necessary access: each role should only access what it needs [2]
HIPAA-aligned privacy training and workflows [3]
Vendor business associate agreements (when needed)
A simple incident response plan (who to notify, what to document)
If you’re considering a contractor clinician group practice, classification matters. The IRS emphasizes evaluating behavioral control, financial control, and the overall relationship. [1]
🔒 Key takeaway: Standardize privacy, access, and documentation before you add more logins and more risk.
Compensation Models and Expectations (Set These Early)
Splits, flat rates, tiered incentives - how to choose
Different models send different signals:
Percentage split works when the practice provides marketing, admin, systems, and support.
Flat rate is simple, but you need forecasting and clear expectations.
Tiered incentives can work, but only if metrics are transparent and fair.
What you expect from clinicians (and what you provide)
To prevent confusion, put expectations in two columns.
What you expect (examples): documentation timelines, consult participation, scope boundaries.
What you provide (examples): onboarding, templates, escalation pathways, marketing support, and consult structures.
Avoiding resentment with transparency
Misconception #3: “We’ll keep it flexible and figure it out.” Flexibility without clarity becomes inconsistency. Put the hard stuff in writing: fees/payout timing, cancellation handling, how changes happen, and how feedback works.
🤝 Key takeaway: Clarity is kinder than flexibility that changes week to week.
Recruiting and Onboarding That Doesn’t Create Chaos
Write a role that attracts self-starters (not passive waiters)
Be specific about your population/niches, what support exists (admin, consult, marketing), documentation expectations, and pay model.
If you want a reality-check lens, see: Therapist job red flags (and green flags that actually matter).
An onboarding plan that covers systems + culture
Onboarding therapists is easier when it’s repeatable. Cover systems (EHR basics, templates, billing workflow) and culture (consult norms, boundaries, how you talk about clients). A simple 30-60-90 plan is often enough.
How to support caseload-building without overpromising leads
New clinicians need support - not guaranteed referrals. Share realistic ranges, offer a 30-90 day ramp plan with checkpoints, and teach how referrals arrive (SEO, networking, niche pages).
Two internal reads that set expectations well:
🌱 Key takeaway: Promise support and a ramp plan, not guaranteed leads.
Culture and Clinical Quality at Scale
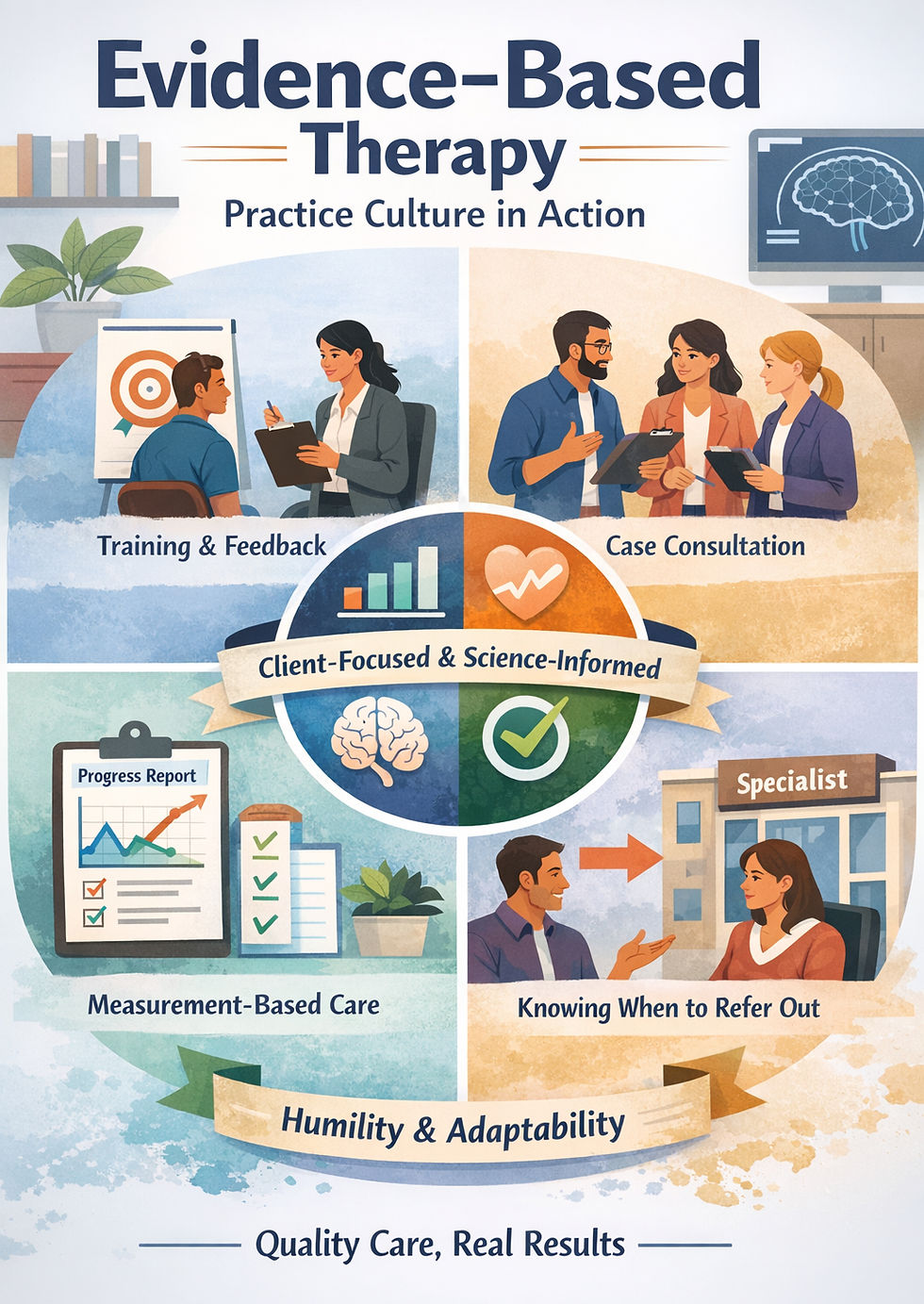
Consultation structures that keep standards high
Culture is built in repeatable places: consult time, documentation review, and how you handle scope and risk. Professional ethics emphasize confidentiality, competence, and appropriate consultation. [5,6]
Simple options: weekly case consult, clear “when to consult” triggers, and light documentation spot-checks for consistency.
Neurodiversity-affirming, shame-reducing tone as a cultural norm
Team culture isn’t a vibe - it’s norms. If neurodiversity-affirming care matters to you, operationalize it: separate a person from a symptom, treat avoidance as information, and build consent and collaboration into plans.
For one example of how this tone can be described publicly, see: Neurodivergent-affirming therapy in Tennessee.
How to handle mismatches respectfully and quickly
Even with strong hiring, mismatches happen. Address issues early with specific examples, a short support plan, and a respectful off-ramp if it’s not improving.
🧩 Key takeaway: Address misfit early, with kindness and documentation, to protect clients and your culture.
The “Platform” Alternative: Grow a Team Without Building Everything
Shared infrastructure that lets you focus on leadership
Sometimes the barrier isn’t vision - it’s build capacity. A platform model can provide shared infrastructure (admin, systems, marketing, consult culture) so you can focus on leadership and clinical standards.
Contact us if you want a runway to build within a platform
If you’re exploring start a group practice Tennessee options and want a runway to build inside established infrastructure, visit Careers at ScienceWorks. We'd love to hear from you!
Summary
Hiring is a leadership decision, not just a staffing decision. Build your policies, workflows, and consultation structure first. Then hire with clarity about expectations, compensation, and culture so growth feels steady instead of chaotic.
About ScienceWorks Behavioral Healthcare
ScienceWorks Behavioral Healthcare is a Tennessee-based behavioral health practice providing therapy, assessments, and coaching with a neurodiversity-affirming, shame-reducing approach. We support clients across the lifespan and partner with clinicians who value ethical practice, strong consultation, and sustainable systems.
References
Internal Revenue Service. Independent contractor (self-employed) or employee? [Internet]. IRS; [cited 2026 Feb 2]. Available from: https://www.irs.gov/businesses/small-businesses-self-employed/independent-contractor-self-employed-or-employee
U.S. Department of Health & Human Services. Minimum Necessary Requirement. [Internet]. HHS; 2013 Jul 26 [cited 2026 Feb 2]. Available from: https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/minimum-necessary-requirement/index.html
U.S. Department of Health & Human Services. Summary of the HIPAA Privacy Rule. [Internet]. HHS; 2025 Mar 14 [cited 2026 Feb 2]. Available from: https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/index.html
Tenn. Comp. R. & Regs. 1180-01-.06 Patient Records. [Internet]. Cornell Law School Legal Information Institute; [cited 2026 Feb 2]. Available from: https://www.law.cornell.edu/regulations/tennessee/Tenn-Comp-R-Regs-1180-01-.06
American Counseling Association. 2014 ACA code of ethics. [Internet]. ACA; 2014 [cited 2026 Feb 2]. Available from: https://www.counseling.org/docs/default-source/default-document-library/ethics/2014-aca-code-of-ethics.pdf
American Psychological Association. Ethical principles of psychologists and code of conduct. [Internet]. APA; [cited 2026 Feb 2]. Available from: https://www.apa.org/ethics/code
Disclaimer
This article is for informational purposes only and is not legal, tax, financial, or clinical advice.