Questions to Ask an I‑CBT Therapist Before You Start OCD Treatment
- Kiesa Kelly

- Dec 3, 2025
- 7 min read

People often tell us, “I’m scared to pick the wrong therapy and make things worse.” That’s understandable. This article explains what to ask an I-CBT therapist (also called Inference‑Based CBT) before you begin OCD treatment - so you can feel informed, respected, and ready. You’ll learn how to evaluate training and experience, treatment planning, safety and consent, support for neurodivergence, and the logistics of online care in Tennessee.
🧠 Key takeaway: You’re the expert on your life; your therapist is the expert on process. The best outcomes happen when both kinds of expertise are valued (4, 5).
Why It’s Okay to Interview Your I‑CBT Therapist
You’re allowed to ask questions and take your time
You’re choosing a partner in your health. Interviewing a prospective clinician isn’t rude—it’s wise. It’s also consistent with measurement‑based, collaborative care like our Comprehensive Therapy Services, where clear goals and shared decisions are the norm.
🧭 Key takeaway: A respectful therapist will welcome your questions, offer straight answers, and encourage you to compare options.
How fit, safety, and trust affect OCD treatment outcomes
Therapeutic alliance—the sense that you and your therapist are working together—predicts outcomes across approaches (4). This is true in person and, more recently, via telehealth (5). Translation: feeling safe and heard is not fluff; it’s evidence‑based.
🤝 Key takeaway: Strong alliance + a sound method (I‑CBT or ERP) is a reliable recipe for progress (1, 3–5).
Questions About Their Training and Experience
“How much experience do you have with OCD and I‑CBT?”
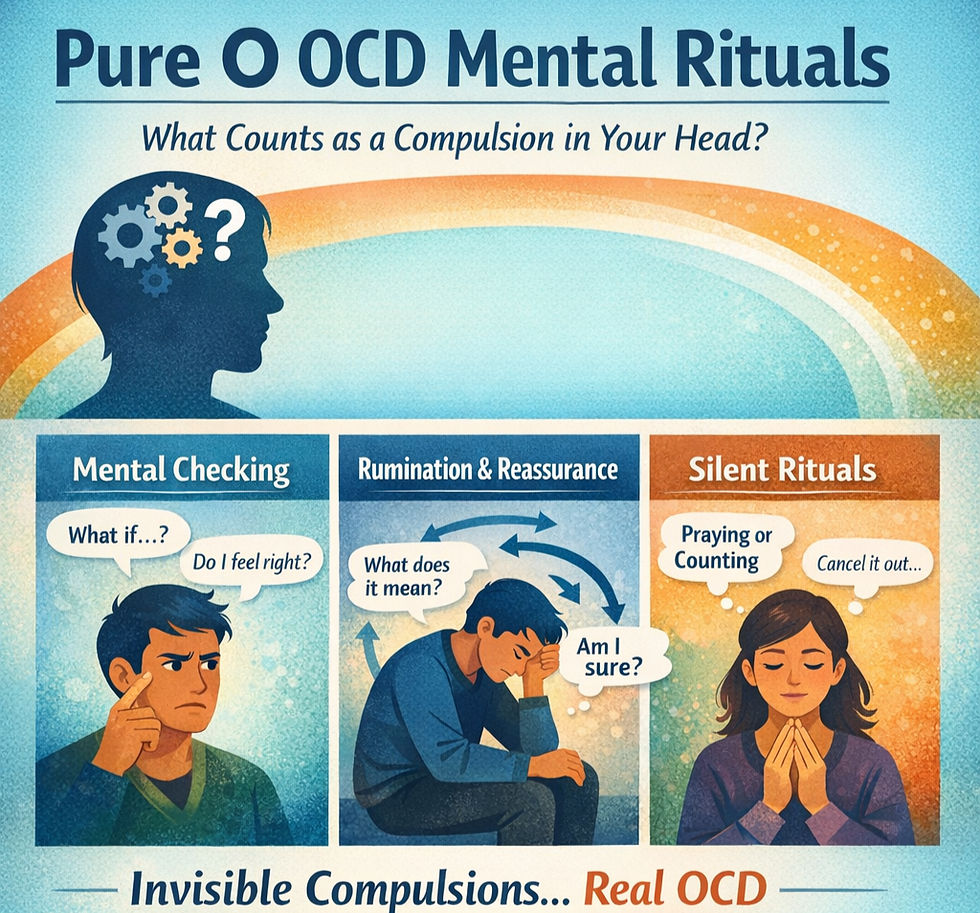
Look for specifics: number of OCD cases treated; common OCD themes they’ve worked with (contamination, harm, religious/scrupulosity, relationship doubts, taboo intrusions, “just‑right”/symmetry, mental compulsions); and experience with both I‑CBT and ERP. I‑CBT targets the reasoning errors ("inferential confusion") that launch obsessional doubt (2), while ERP changes the learn‑by‑doing patterns that keep compulsions going (3).
🔎 Listen for: real‑world examples of how they adapt interventions to your theme and your day‑to‑day life.
“What training or supervision have you had in I‑CBT?”
Ask about formal coursework, mentorship, and consultation with I‑CBT‑trained supervisors. Bonus points if they can describe how they assess “inferential confusion” and track change across sessions (2).
Clarifying whether they also use ERP and other approaches
Evidence shows ERP is effective for OCD (3), and I‑CBT has RCT evidence as an effective alternative that can be preferable for some (e.g., with overvalued ideas) (1, 2). Many people benefit from both—for example, I‑CBT to de‑fuel obsessional doubt and ERP to retrain rituals. Ask how they decide when (and how) to use one, the other, or an integration.
Questions About Their Treatment Approach
“How do you explain I‑CBT in everyday language?”
You should hear something like: “OCD starts when the brain treats a possibility as if it were true. I‑CBT helps you catch that leap, return to ‘senses + common sense,’ and step out of the OCD story.” That’s I‑CBT in plain English and aligns with the research (2). For a gentle overview of ERP, see how ERP actually works in practice.
🧩 Key takeaway: I‑CBT targets the start of the OCD loop (doubt/inference). ERP targets the cycle (exposure + not ritualizing). They can complement each other (1–3).
“How will we decide whether I‑CBT, ERP, or both are right for me?”
Ask how they assess themes, compulsions (including mental rituals), conviction/overvalued ideas, and any trauma or insomnia that might change pacing. Sometimes a brief psychological assessment clarifies whether OCD is present and what to treat first.
“How do you plan and track treatment goals?”
Look for:
Clear, shared goals (e.g., reduce reassurance seeking from 20/day to 5/day)
Regular symptom measurement (e.g., Y‑BOCS, distress ratings, functional goals)
Session‑to‑session check‑ins and adjustments
A written plan for relapse preventionThat’s standard in our OCD care and across our practice.
Questions About Safety, Consent, and Pacing
“What happens if something feels too fast or overwhelming?”
You deserve transparent options: slowing down, adding skills (e.g., attention‑shifting or values‑based actions), or switching tools (e.g., pausing ERP to strengthen I‑CBT reasoning first). Good therapists support consent and choice at every step.
“How do you handle topics that feel very shameful or scary?”
OCD loves to whisper “don’t tell” about taboo themes. A skilled clinician will normalize the territory and keep you safe while still doing effective work—never using shock or humiliation. If you’re curious how we approach exposure humanely, see our gentle introduction to ERP.
“How do you include me in decisions about next steps?”
Ask how they gather your feedback, how often they review progress data, and how they decide to continue, pause, or switch approaches. Shared decision‑making strengthens alliance and outcomes (4, 5).
🛟 Key takeaway: You can (and should) call time‑outs, ask for rationale, and co‑design the next step—no surprises.
Questions About Working with Neurodivergence and Complex Situations
“Do you work with autistic/ADHD clients or demand avoidance?”
If you’re neurodivergent, it helps to work with a team fluent in autistic and ADHD presentations and in the ways these overlap with OCD. Our practice is neurodivergent‑affirming and offers integrated executive function coaching alongside therapy, which many clients find stabilizing.
“How do you adapt I‑CBT if standard homework doesn’t fit?”
Flexibility is a feature, not a bug. Good I‑CBT clinicians tailor reasoning exercises to your sensory profile, energy, and schedule. Examples: shorter, more frequent reps; visual supports; values‑anchored action steps; asynchronous check‑ins. Many clients appreciate that I‑CBT can feel less threatening than ERP at first—yet still evidence‑based (1, 2).
Practical Questions: Logistics, Cost, and Access
Scheduling, fees, and insurance details
Clarify session length and cadence; fees; out‑of‑network support; sliding‑scale options; and whether Tennessee in‑network benefits apply. We outline ours on Comprehensive Therapy Services and encourage transparent, up‑front estimates.
Telehealth options and how online I‑CBT works
Telehealth I‑CBT/ERP is effective for many people (including adults and teens) and can reduce access barriers (1, 3, 6). If you’re searching for an ICBT therapist near me or an online ICBT therapist Tennessee, secure video sessions mean “near me” can be your couch—as long as you’re located in TN at the time of service. See our brief guide: I‑CBT for OCD in Tennessee.
What to expect from the first 1–3 sessions
Session 1: History, goals, and a clear map of your OCD cycle; plan immediate relief steps that don’t feed compulsions
Session 2: Personalized I‑CBT framework; begin reasoning exercises; set simple, doable between‑session experiments
Session 3: Refine fit and pacing; consider adding ERP or skills; confirm how progress will be tracked and celebratedTo get started or compare fit, you can schedule a free consultation.
What It Might Feel Like When You’ve Found a Good Fit
Feeling informed, not pressured
You’ll know what you’re doing and why. You’ll see how I‑CBT or ERP links to your specific doubts and rituals, and you’ll have a say in pacing and next steps.
Feeling like your concerns are heard and taken seriously
You’ll feel respected, not pathologized. Sessions feel collaborative—less like a test and more like training your brain in real‑world conditions. If you’re looking for an OCD specialist Tennessee, that’s the vibe to look for.
🌟 Key takeaway: Good care is clear, kind, and evidence‑based. You should leave early sessions with a shared plan and small wins.
Quick Checklist: OCD Treatment Questions to Ask
How many OCD cases have you treated with I‑CBT and ERP? (1–3)
What I‑CBT training/consultation do you have? (2)
How will we decide between I‑CBT, ERP, or both? (1–3)
How do you measure progress session‑to‑session? (4)
How do you adapt for autistic/ADHD clients?
What’s the plan if I feel overwhelmed?
How do telehealth sessions work logistically and clinically? (5–6)
Ready to talk with an I‑CBT therapist?
If you’re comparing options or searching “how to choose an ICBT therapist,” we’re happy to help you think it through—even if you decide on another clinic. Meet our team on Meet the ScienceWorks Team or go straight to a free consult.
About the Author
Kiesa Kelly, PhD, HSP is a licensed psychologist and practice owner at ScienceWorks Behavioral Healthcare. She earned her PhD in Clinical Psychology (Neuropsychology concentration) from Rosalind Franklin University and completed an NIH‑funded postdoctoral fellowship at Vanderbilt University. Dr. Kelly has 20+ years of experience with psychological assessment and evidence‑based care, including I‑CBT, ERP, ACT, EMDR, and CBT‑I. Learn more on Kiesa Kelly, PhD.
Dr. Kelly provides telehealth therapy and assessment in Tennessee and multiple additional PSYPACT states. She is passionate about neurodivergent‑affirming care and helping clients build science‑backed, humane plans for relief and growth.
References and Citations
(1) Aardema, F., Bouchard, S., Koszycki, D., Lavoie, M. E., Audet, J.‑S., & O’Connor, K. (2022). Evaluation of Inference‑Based Cognitive‑Behavioral Therapy for Obsessive‑Compulsive Disorder: A Multicenter Randomized Controlled Trial with Three Treatment Modalities. Psychotherapy and Psychosomatics, 91(5), 348–359. https://doi.org/10.1159/000524425
(2) Julien, D., O’Connor, K., & Aardema, F. (2016). The inference‑based approach to obsessive‑compulsive disorder: A comprehensive review of its etiological model, treatment efficacy, and model of change. Journal of Affective Disorders, 202, 187–196. https://doi.org/10.1016/j.jad.2016.05.060
(3) Song, Y., Li, D., Zhang, S., Jin, Z., Zhen, Y., Su, Y., Zhang, M., Lu, L., Xue, X., Luo, J., Liang, M., & Li, X. (2022). The effect of exposure and response prevention therapy on obsessive‑compulsive disorder: A systematic review and meta‑analysis. Psychiatry Research, 317, 114861. https://doi.org/10.1016/j.psychres.2022.114861
(4) Flückiger, C., Del Re, A. C., Wampold, B. E., & Horvath, A. O. (2018). The alliance in adult psychotherapy: A meta‑analytic synthesis. Psychotherapy, 55(4), 316–340. https://doi.org/10.1037/pst0000172
(5) Aafjes‑van Doorn, K., Spina, D. S., Horne, S. J., & Békés, V. (2024). The association between quality of therapeutic alliance and treatment outcomes in teletherapy: A systematic review and meta‑analysis. Clinical Psychology Review, 110, 102430. https://doi.org/10.1016/j.cpr.2024.102430
(6) Vogel, P. A., Solem, S., Hagen, K., Moen, E. M., Launes, G., Håland, Å. T., Hansen, B., & Himle, J. A. (2014). A pilot randomized controlled trial of videoconference‑assisted treatment for obsessive‑compulsive disorder. Behaviour Research and Therapy, 63, 162–168. https://doi.org/10.1016/j.brat.2014.10.007
Additional context: For readers who want more on internet‑delivered CBT/ERP for OCD, see Feusner et al. (2022), J Med Internet Res, 24(5), e36431. https://doi.org/10.2196/36431
Disclaimer: This article is for informational purposes only and is not a substitute for diagnosis, treatment, or medical advice.